Partial Knee Replacement
Overview
The information presented here is similar to that presented in the Total Knee Replacement section. Differences will be italicized .
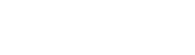
There are three main sections (compartments) of the knee joint, and there are partial (also called “unicompartmental”) knee replacements that exist to resurface each of those compartments:
- Medial Compartment Knee replacements
- Lateral Compartment Knee replacements
- Patellofemoral joint replacements
This article discusses only Medial Compartment Knee Replacements.
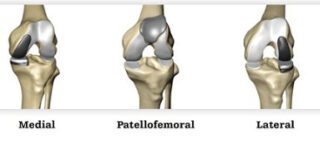
Whereas total knee replacements replaces all compartments in the knee, a partial knee replacement replaces only one compartment. Both total knee replacements and partial knee replacements are designed for patients with severe knee arthritis. A partial knee replacement however, is designed for the subset of those patients that have arthritis in only one compartment.

Frequently Asked Questions
- Am I a candidate for a Partial Knee Replacement?
- Why would someone have a Partial Knee Replacement instead of a Total Knee Replacement?
- Why would someone have a Total Knee Replacement instead of a Partial Knee Replacement?
- How long does a partial knee replacement last?
- What if I can’t choose between a Partial and a Total knee replacement?
- What is Knee Arthritis?
- What non-surgical options are available to treat Knee Arthritis
- When is Knee Replacement Suggested?
- What gets “Replaced” during a knee partial replacement?
- How long am I in Hospital after Partial Knee Replacement?
- Does Partial Knee Replacement Hurt?
- What are the risks of partial knee replacement surgery?
Only a subset of patients that are candidates for total knee replacements are candidates for Partial Knee Replacements.
You may be a candidate for a Medial Partial Knee Replacement if:
- You have severe knee arthritis only in the medial (inner) portion of your knee and
- You have pain mostly around the inner portion (medial) of your knee and
- You don’t have much pain in the front (anterior) portion of your knee and
- You have less than 15 deg “fixed flexion deformity” (your knee straightens out pretty well) and
- Your BMI is less than 40 and
- Your ACL and PCL are intact (can be assessed by your orthopedic surgeon) and
- You don’t have inflammatory arthritis and
- Your orthopedic surgeon thinks you are a candidate for a partial knee replacement
The above criteria have been discussed in the scientific literature. They are not rules. These are not meant to guide the practice of any specific surgeon, but reflect Dr. Cayen’s practice at the time of writing.
- The recovery after partial knee replacement is faster than total knee replacement
- In fact, most of Dr. Cayen’s partial knee replacement patients go home the same day of surgery.
- Patients regain independent mobility (walking without a cane or crutch) in about half the time, compared to total knee replacement
- The pain after partial knee replacement is less than after total knee replacement
- It is Dr. Cayen’s experience (and scientific literature suggests) that patients enjoy their knees more after Partial Knee Replacement, compared to Total Knee replacement.
- After recovery from partial knee replacement, patients feel that they have more of a “natural knee”, compared to Total Knee Replacement
- The function of a partial knee replacement is better than that of a total knee replacement.
Remember: Only a subset of patients that are candidates for total knee replacements are candidates for Partial Knee Replacements.
- Data from various National Registries suggest that a partial knee replacement lasts less time than a total knee replacement. This data suggests that patients with partial knee replacements need knee revision surgery sooner than patients who have total knee replacements.
- Cohort data (that is data taken from a single group, rather than from an entire country) demonstrates that 95% of total knee replacements last 10 years while 90% of partial knee replacements last 10 years.
- Data from various National Registries suggest that a partial knee replacement lasts less time than a total knee replacement. This data suggests that patients with partial knee replacements need knee revision surgery sooner than patients who have total knee replacements.
- Cohort data (that is data taken from a single group, rather than from an entire country) demonstrates that 95% of total knee replacements last 10 years while 90% of partial knee replacements last 10 years.
That is completely normal. Dr. Cayen usually guides patients through that decision during their consultation.
The knee joint consists of the connection (articulation) between the end of the thigh bone (distal femur), top part of the leg bone (proximal tibia) and the undersurface of the knee cap (patella). Arthritis is when the cartilage covering any one of those surfaces wears away. When the underlying bone starts to rub, this causes the pain associated with arthritis.
Patients with knee arthritis often feel
- knee pain with standing or walking for long periods of time
- knee stiffness limiting their ability to
- straighten the knee during walking or
- fully bending the knee while sitting in low chairs or on the floor.
Knee Arthritis can be caused by
- Osteoarthritis (wear and tear with age or obesity)
- Rheumatoid arthritis or other inflammatory arthritis
- chronic ACL tear (remote sports injury)
- previous fractures or other trauma around the knee
- Previous knee infection
The initial treatment for knee arthritis can include
- Pain medication – unless you have liver problems, acetaminophen (Tylenol) is typically recommended, to start. Many medical associations have recommended AGAINST using narcotics for arthritis pain, as this can risk addiction, without an improvement in pain.
- Anti-inflammatory medication – ask your family doctor if you may safely take anti-inflammatory medication. Patient with a history of stomach ulcers, high blood pressure, or kidney disease should usually avoid these types of medication.
- Physiotherapy – visit a physiotherapist so that they can teach you a program focused on quadriceps, hamstrings and abductor strengthening that you can do at home on your own. See your physiotherapist occasionally so that they can monitor your progress, correct your form, and add exercises to your program. Even if you end up proceeding to knee replacement surgery, “Pre-hab” will help quicken your postoperative recovery. If you are being funded by extended health benefits and you are on a waitlist for surgery, be sure to save most of your benefits for after surgery.
- walking aids – a cane or walker may help walking be more comfortable
- knee injections – a good non-operative option. see section on injections
- Weight-loss, if necessary. If you are overweight, losing as little as 20 pounds can improve your knee pain. Although exercise is important for strong muscles and heart health, diet is by far more important for weight loss. Speak to your family doctor about diet resources. You can get started with information regarding healthy eating at the Heart and Stroke Foundation of Canada
- Bracing – A custom made offloading brace can sometimes help with the pain while walking. Dr. Cayen recommends braces that are tailored to each patient (custom made), rather than ones that can be bought off the shelf. Braces are expensive, but are often covered under extended health benefits. Braces can also be bulky and may not fit all leg shapes well.
If non-surgical treatment does not adequately manage symptoms then total knee replacement can be considered.
No amount of online information can replace a visit with an orthopedic surgeon to determine if you would benefit from a knee replacement. This serves as a guide only. Knee replacement is an option in patients who have evidence of knee arthritis and
- knee pain due to the arthritis that significantly limits walking or other everyday activities. Knee arthritis is only one of the many causes of pain around the knee. (Other causes of knee pain include back issues, tendon, muscle, or other soft tissue problems.)
- tried non-surgical options that have not adequately helped with the pain/function
- good underlying health. Patients who have had recent cardiac events, heavy smokers, poorly controlled diabetes, morbid obesity or dementia, are at high risk for complications after knee replacement surgery.
- Can commit to the physiotherapy program after surgery.
In knee replacement surgery, your surgeon fits a metal cap to the end of the thigh bone (distal femur) and top part of the leg bone (proximal tibia). A piece of plastic (polyethylene) is placed in between these two components. With partial knee replacement, only the inner surfaces (medial femoral condyle and medial tibial plateau) are replaced. The incision is made in the front of the knee.
Most patients go home the same day of surgery. You will need crutches or a walker initially.
In short, yes, but less than a total knee replacement. During the surgery itself, you won’t feel anything though (see Day of Surgery below). Dr. Cayen also uses lots of local anesthetic during the procedure to help keep you comfortable. Dr. Cayen also recommends cryotherapy (an ice-machine) to help with pain control after surgery (See Preparing for Surgery Below). Knee replacement surgery however is more painful than hip replacement surgery, and the recovery is slower.
Arthritis developing in another part of the knee
It is possible that as you age, you may develop arthritis in a part of your knee that wasn’t replaced by the partial knee replacement. This may contribute to the slightly higher revision rate in partial knee replacements compared to total knee replacements. Data suggests that 95% of total knee replacements last 10 years while 90% of partial knee replacements last 10 years.
Infection
The lifetime risk of a serious infection after a knee replacement is approximately 1%. Some of these infections occur soon after surgery, but most occur months or years afterwards. The treatment for serious (deep) infections includes revision surgery and IV antibiotics. Skin infections (cellulitis) after knee replacement is more common and can be treated with oral antibiotics.
People at higher risk for infection include patients with poorly controlled diabetes, patients with morbid obesity (BMI more than 40), patients who are immunocompromized (eg HIV, lymphoma), or are taking immunosuppressant drugs, patients with peripheral vascular disease (poor circulation to hands and feet) and smokers. An ongoing infection at the time of surgery from another source (eg active urinary tract infection, tooth abscess, diabetic foot infection can increase your risk of infection after surgery.
In order to prevent infection, your surgeon will give you one dose of antibiotics through your IV in the operating room before your surgery. You will get one more dose after your surgery. Growing evidence suggests that numerous doses of antibiotics after your surgery does not prevent infection.
The symptoms of infection include fevers, redness around the wound, persistent leaking from the wound, increasing pain in a previously well-functioning joint replacement. If you think you are developing an infection around your knee replacement, call your orthopaedic surgeon’s office as soon as possible or go to your nearest emergency department.
Skin Numbness
Most patients experience a patch of skin numbness, about the size of their palm just to the outside of (lateral to) the incision site of the knee replacement scar. This patch of skin numbness can decrease in size over months to years, but will not affect your function.
Incomplete pain control
Knee replacement can help with 80-85% of knee pain associated with arthritis after 3 months of recovery, but doesn’t usually get rid of 100% of knee pain. Most people still get some aches and pains in their knee replacement, even after recovery is complete.
Knee stiffness
Immediately after total knee replacement, your knee will be stiff and painful to move. It is of the utmost importance to work on moving your knee despite this discomfort in the first few days after your knee replacement. Doing the exercises given to you by your physiotherapist immediately after your surgery will help you enjoy your knee replacement in the long run. If you do not work on bending and straightening your knee after your surgery, your knee replacement can become permanently stiff. Ideal range of motion after knee replacement recovery is 0 (completely straight) to 120 degrees. After surgery, it is unlikely you will be able to squat all the way down such that your heel touches the back of your thigh.
Blood Loss
Some blood loss during knee replacement is normal. Blood loss requiring a blood transfusion after surgery is rare unless you are anemic (low hemoglobin levels) before surgery. You will be sent for blood work when you book your surgery to make sure that you are not anemic. If you are anemic before surgery, we will refer you to our Patient Blood Management Coordinator who may suggest ways to build up your hemoglobin levels prior to your surgery. The risk of requiring a blood transfusion increases if you are having both your knees replaced at once.
Blood Clot
Blood clots in leg veins can occur after knee surgery. Your surgeon will prescribe a medication for you to take after your surgery in order to prevent blood clots. If a clot develops in a deep leg vein (deep vein thrombosis – DVT) above the knee, it will need to be treated with stronger blood thinners. Above knee DVTs need to be taken seriously because they can cause clots that go to the lungs (pulmonary embolus), which is a very serious condition. If you have previously had a DVT, please let your surgeon know prior to your surgery.
Component loosening
The metal components of the knee replacement are usually cemented to your bone during a knee replacement. Over the years however, the bond can loosen, requiring a revision of the components. Less common causes of early loosening include infection, morbid obesity and severe osteoporosis.
Damage to Blood Vessels or Nerves
Damage to major blood vessels or nerves causing permanent muscle weakness or compromised blood flow to the leg is exceptionally rare.
Navigating the System
Appointments Before Knee Replacement
- Family Doctor
If you are wondering if you need a knee replacement, the first step in the Canadian Health Care System is to see your family doctor. Your family doctor will ask you questions, do a physical exam and order x-rays, if they think it’s necessary. If your x-rays show arthritis, and you are interested in a knee replacement, then your family doctor can refer you to an orthopaedic surgeon, like Dr. Cayen, who performs knee replacements. You can request that your family doctor refer you to an orthopaedic surgeon of your choice.
- Central Intake Clinic
For patients living in Ontario, Dr. Cayen’s hip and knee arthritis referrals are fast-tracked to a Central Intake Clinic, where patients are initially seen by an Advanced Practice Physiotherapist (APP). The APP will perform a physical exam, review x-rays with you and educate you about knee replacements, if you’re a candidate. The APPs can not make the determination if you are part of the subset of total knee replacement patients that is also a candidate for a Partial knee replacement. If you are interested in knee replacement in general and are a candidate, you will then have an appointment made with Dr. Cayen, usually on a different day. Although seeing the APP might seem like an extra step, the feedback we get from patients is that patients learn a lot about the procedure during that visit and find it helpful. Dr. Cayen reserves slots for patients who have been seen by the APP, so the wait to see him from the time of the initial referral from the family doctor (Wait 1) is not lengthened in the process.
- Dr. Cayen
When you see Dr. Cayen, he will ask you some questions about yourself, review your medication list, perform a physical exam on your knee and review your x-rays. If you, together with Dr. Cayen decide to proceed with knee replacement, you will sign consent for surgery, attesting that you understand the risks and benefits of surgery. You will then complete some blood work, if it has not already been done recently (CBC, electrolytes, Creatinine, Vitamin B12, Iron panel). Dr. Cayen’s Administrative assistant will call you over the subsequent 2-3 weeks to discuss your surgical date. You may ask Dr. Cayen’s Administrative assistant to be placed on a “cancellation list” if you are able to go ahead with your surgery on short notice.
- Surgical Pre-Screening
You will have a Surgical Pre-Screening Appointment at the Hospital up to 1 month prior to your surgery. There, you will see a nurse who will review your medications (please bring them with you). You will also see an anesthesiologist. You may also see a physiotherapist. You should have a discharge plan in place prior to your surgical pre-screening appointment.
- Internal Medicine
A separate Internal Medicine appointment may be necessary. We will let you know if that is the case.
- Your other Treating Physicians
You may need to follow up with your family doctor or your other treating physicians (endocrinologist, cardiologist, rheumatologist, if you have one) prior to your surgery to discuss your suitability for an elective knee replacement or to discuss changing or temporarily stopping some of your medications prior to surgery.
Preparing for Surgery
- Discharge Planning
Our patients at Humber River Hospital who undergo partial knee replacement are discharged home the same day of surgery. Patients are encouraged to start discharge planning as early as possible in the process (even before they meet Dr. Cayen).
You must plan to be discharged from hospital to a place where someone can help you the evening of surgery, and for the subsequent 2 to 3 days. You may be discharged back to your own home or to a family member or friend’s place after surgery, as you have arranged. You should let Dr. Cayen know your discharge plan during your visit with him.
If you do not have a place where you can be monitored after your surgery, you may choose to consider respite care at a short-stay retirement home. Respite care must be arranged by you well in advance of the surgery date. Respite care is an out of pocket expense. A sample list of respite care locations can be found here.
For final questions regarding your discharge planning, you may ask to speak with a Social Worker or our Orthopaedic Care Navigator.
- Do I Continue my regular Medications?
Do not stop or change any medications before speaking with your doctor. The information below is meant only to give you an idea of what to expect before your surgery.
Inflammatory Arthritis Medications
If you are taking medications for inflammatory arthritis (such as Rheumatoid Arthritis), you may need to stop some of those medications for a few weeks before and after your surgery. Many Disease Modifying Antirheumatic Drugs can increase the risk of infection around the time of surgery and can seriously affect wound healing. Let Dr. Cayen know if you are taking any such medications. You will need to speak with your Rheumatologist before stopping these medications temporarily. A scientific review paper accessible by your Rheumatologist can be found here.
Blood Thinners
If you are taking blood thinners by mouth, you may need to stop taking those for up to a week prior to your surgery. Let Dr. Cayen know if you are taking any such medications. You will need to speak with your Family Doctor before stopping these medications temporarily.
Diabetic Medications
If you have diabetes, you will be seen by an internal medicine specialist prior to your surgery who will tell you which of your diabetes medications should be changed temporarily prior to your surgery. You may need to speak with your Family Doctor or Endocrinologist before adjusting your medications temporarily.
Narcotics
If you are taking narcotics for chronic knee pain or other chronic musculoskeletal pain, Dr. Cayen suggests that you work with your prescribing physician to slowly lower or eliminate the use of those medications. Patients who are taking narcotics prior to surgery have a more challenging course with pain control after surgery.
- Information for patients on opioid tapering can be found here.
- Information for physicians regarding opioid guidelines can be found here.
- General Health
Weight Control and Diet
- Being overweight can put excessive forces through knee replacements and may lead to early loosening of the implants. Scientific data suggests that if your Body Mass Index (BMI) is more than 40, you are at increased risk of infection after knee replacement. Excessive weight can compromise optimal component position during surgery. Decreasing your weight, if necessary can improve your knee pain prior to surgery and improve the speed of recovery after surgery.
- Calculate your BMI here
- Although exercise is important for weight control, diet is by far more important. Some things you can do to help with your diet include lowering overall portions, eating food high in protein and lower in carbohydrates, not eating after dark, not drinking beverages with calories (such as soft drinks or fruit juices) and creating a food diary. Speak to your family doctor about a weight loss program, if necessary. One resource for weight loss from the Heart and Stroke Foundation can be found here.
Smoking
Stop smoking at least 6 weeks prior to your surgery. In addition to damaging your lungs and heart, smoking slows bone healing which is an important part of having the implants in joint replacement surgery bond to your bone. Smoking will make your recovery from surgery take longer. Smoking also increases the risks of poor wound healing and increases the risks of infection. Resources for smoking cessation can be found here.
Diabetes
If you have diabetes, getting your blood sugars under control prior to your surgery is important. Before your surgery, speak to your family doctor or endocrinologist about your “Hemoglobin A1c”. If it is high, it might mean that your blood sugars are not under control. Poorly controlled diabetes increases the risk of infection after knee replacement surgery.
Strengthening Exercises
Seeing a physiotherapist once or twice before your surgery to teach you quadriceps-strengthening exercises may be helpful to quicken your recovery after surgery. The stronger you are before your surgery, the stronger you will be afterwards and the faster your recovery will be.
- Assistive Devices
- 2-wheeled walker or crutches will be needed for 1-3 weeks after your surgery.
- Cane. – You will progress to using a cane after the walker/crutches. You may need a cane until the 6-12 week mark.
- Non-slip bath mat
- Dr. Cayen recommends the use of a cold-compression device (cryotherapy) for pain control after your surgery. This may be covered by many extended-health insurance policies. Dr. Cayen’s administrative assistant will speak to you about cryotherapy prior to your surgery.
- Day of Surgery
Do not eat or drink anything after midnight the night before surgery. You should take the medications you have been instructed to take the morning of surgery with sips of water. Do not take the medications you have been told to stop taking.
Arrive at the Hospital 2 hours before your scheduled surgery. You will be registered, then get changed into a gown. You will have an intravenous line started and may be give some medications for pain and nausea. You will then see our anesthesiologist who will discuss the anesthetic. Typically, knee replacements are done with a spinal anesthetic in addition to nerve blocks in the leg. Once in the operating room, you are given sedation through your IV, such that you are sleepy but no breathing tube is required.
Recovery
- Initial Recovery
You will wake up and recover initially in the Post Anesthetic Care Unit (PACU) where xrays of your new knee will be taken.
You will then be moved to our Surgical Day Care (SDC), where you will complete your recovery, receive some medications and be seen by our physical therapists (PTs). Our PTs will get you up walking in the SDC within a few hours of your surgery. If you will be going home with a Continuous Adductor Canal block.
You will be allowed to put full weight on your leg after surgery. When our phyiotherapists deem your safe for discharge home and your pain and nausea are under control, you will be discharged home with family or friends as you have arranged. You must arrange to get a ride to and from your surgery.
You will be discharged home with prescriptions for pain killers, a stool softener (if needed) a blood thinner and a prescription for post-operative physical therapy.
You may need a walker or crutches for 2-3 weeks after your surgery. You may need to use a cane up to the 6-12 week mark after your surgery. Everybody’s recovery pace is different. As long as you are improving week-to-week, you are doing well. Most of your recovery should be complete around the 3 month mark, although people do continue to improve beyond that time.
- Physiotherapy after Surgery
The success of a knee replacement is highly dependent on the physiotherapy you do after surgery. Your physiotherapist will teach you exercises that you will need to do at home. These include quadriceps strengthening as well as knee range of motion exercises. It is crucial that you do these exercises at home, despite the discomfort. Some of these exercises can be printed here
- Follow-up After Your Surgery
You will see Dr. Cayen 1-2 weeks after your surgery in the Fracture Clinic. He will check your wound and make sure you are doing your home exercises. Dr. Cayen will check how well you can bend and straighten your knee, and see if you can do a straight leg raise. Your staples will be removed. Your subsequent two follow-ups with Dr. Cayen will be at approximately the 6 week and the 3-4 month mark after your surgery in the Fracture Clinic. If you are feeling well at that point, no further follow up with Dr. Cayen is necessary unless concerns arise. If you have concerns regarding your knee replacement, please give Dr. Cayen’s Administrative Assistant a call.
- Wound Care
Before you leave the operating room, Dr. Cayen will place a water-proof bandage over your incision. You can shower with this bandage on. You will be instructed to take this bandage off 7 days after your surgery. More information about the dressing can be found here. You may replace the bandage with a strip dressing for showers, in order to keep the wound dry until the wound heals completely. Do not submerge the wound under water in a tub or swimming pool until the wound is completely closed (usually around 3 weeks after surgery).
- Driving
For right-leg surgery, you can drive once you are not using walking aids and are not using narcotics for pain control.
For left-leg surgery, if you are driving an automatic transmission vehicle, you can drive once you are no longer taking narcotics for pain control. If you drive a standard transmission vehicle, the restrictions are similar to right-leg surgery.
You need to feel confident that you can hit the break with good force and reaction time before you return to driving.
- Work and Activities
Work
Return to work depends on the kind of job you have.
Sedentary/Desk job: It is reasonable to take 6 weeks off of a sedentary job after knee replacement. Many patients start working from home after a 2-3 of weeks (as long as they are not taking narcotics for pain). Dr. Cayen suggests working not more than 2-3 hours per day during the first few weeks after surgery and to take frequent breaks. Sitting for long periods of time after joint replacement surgery can theoretically increase the risk of blood clots. Spend your first few weeks after surgery doing your physiotherapy and resting.
Walking Jobs: Typically patient can get back to an active job approximately 2-3 months after surgery. When you do return to work, Dr. Cayen suggests return to work gradually, with graduated hours and graduated duties over a number of weeks.
Manual labour: Historically, joint replacement surgery was reserved for the elderly and certainly those people who were not doing manual labour jobs. We do not have long term data on the effects of manual labour on joint replacement surgery however heavy lifting does place large forces through the joint. This could possibly lead to early loosening. Dr. Cayen does not recommend returning to a job requiring heaving lifting after joint replacement. If your are currently able to perform your duties in a job requiring heavy lifting, perhaps a joint replacement is not right for you at this time. You might want to hold off on joint replacement until after you are no longer able to perform heavy lifting, or discuss with your orthopaedic surgeon.
Activities
Most patients experience an improvement in their daily activities after their rehabilitation from knee replacement surgery. You are encouraged to resume non-impact activities after your recovery. This can include, walking, cycling, elliptical training, swimming and golf. Many patients have returned to light tennis, skiing and even non-contact ice hockey/skating after their rehab is complete. As a general guide, if you can perform these activities without the risk of falling or loosing control (ie an expert hockey player or skier who takes it easy) before surgery, then you may train and eventually return to that activity. Before you return to sport, it is imperative that your physiotherapist or athletic therapist guides your return to activity with a sport-specific exercise regimen, lest you risk injury.
It is not recommended that you return to high impact activities like jogging, running or jumping sports after joint replacement. Such activities cause high forces through the joint and can theoretically lead to early loosening of the components.
- Dentist
For dental procedures, you do not need extra antibiotics above what is normally prescribed by your dentist. You should be in optimal dental health prior to your knee surgery. Infected teeth should be treated fully prior to your knee surgery. If you are approaching your scheduled regular dental cleaning, have that done prior to your knee surgery. Continue on your regular dental cleaning schedule after your knee surgery.
The Canadian Arthroplasty Society consensus statement for patients with total joint replacements having dental procedures can be found here. You may show this to your dentist.
- Travel and the Airport
Travel
Vacation travel after knee replacement can be done as soon as 6 weeks post operatively. Although it is possible to travel before then, it is recommended that they be short flights and that you get up out of your seat hourly to move.
For those who must travel prior to 6 weeks after surgery, blood thinner medication may be recommended and can be discussed with Dr. Cayen or your family doctor.
Note that your recovery and self-directed physiotherapy program should continue until approximately the 12-week mark.
Metal detectors at the airport
You may set off metal detectors at the airport. You do not need a note from Dr. Cayen or your family doctor regarding your joint replacement. Just let the security personnel near the metal detector know. They may ask you to go through the body scanner instead. Given how common joint replacements are, security personnel are accustomed to this issue.
A video on metal detectors with joint replacements from the American Association of Hip and Knee Surgeons can be found here.
DISCLAIMER: The information on this website is intended to help current and prospective patients of Dr. Cayen understand joint disease as well as treatment options available. It is also meant to provide background information to prospective patients such that their visit with their doctor is most helpful. This website is not meant to provide specific medical advice, treat or diagnose any medical condition. It is not meant to take the place of a visit with your doctor or Dr. Cayen.
About Dr. Cayen
Dr. Barry Cayen is an orthopedic surgeon at Humber River Hospital, specializing in adult hip and knee replacements, sports surgery of the knee, and trauma. He performs Total Hip Replacement Surgery using the Direct Anterior approach with a Hana table.