ACL Tears and Reconstruction
Overview

Frequently Asked Questions
- What are ACL Tears?
- What are the treatment options for ACL Tears?
- What is ACL Reconstruction?
- Physiotherapy after ACL reconstruction
- What are the risks of ACL reconstruction surgery?
Anatomy
The Anterior Cruciate ligament (ACL) is one of the main stabilizing ligaments of the knee. The ACL is one of the ligaments connecting your tibia and Femur. Other ligaments include the Lateral Collateral, Medial Collateral and Posterior cruciate ligaments (LCL, MCL and PCL respectively) but are not the topic of this article.
Cause
People who have ACL tears typically remember an incident when they landed or twisted their knee awkwardly while performing a high-energy activity (eg soccer, basketball, hockey, rugby, landing from a jump etc). Usually the patient is unable to finish the game or activity, and the knee swells up within a few hours.
First Aid
After an ACL tear, it is important that you do your best to decrease the swelling by icing the knee (either using Ice packs or a cryo-compression unit). Never place ice directly against the skin. Never fall asleep with ice on you. A good rule of thumb is 20 minutes on, 20 minutes off. You may need crutches for the first few days after such an injury.
Diagnosis
Xrays are normal with isolated ACL tears. The diagnosis of an ACL tear is made from a combination of the physical exam performed by your doctor and an MRI. It is difficult for your doctor to properly examine your knee if it is very swollen, so decreasing knee swelling as soon as possible is better for your comfort and helps your doctor figure out what’s wrong.
Natural History
ACL tears do not heal by themselves. Some tears can be incomplete and may not cause significant instability. Most traumatic complete tears of the ACL in young people cause significant knee instability.
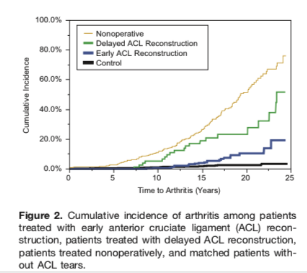
Data suggests that ACL tears in young people cause knee arthritis later in life. If you’re young, having your ACL reconstructed may slow the progression of knee arthritis, but does not prevent knee arthritis outright. One study of patients with an average age of 28 (see graph below) suggests that people treated without surgery after ACL tears (yellow line) have a much higher risk of developing arthritis compared to people who did not have ACL tears (black line). The risk of developing arthritis is lowered if people with ACL tears have reconstructive surgery (blue line). ACL reconstructive surgery looses some of its protective effect if reconstruction is delayed by over one year. So if you’re young and you have an ACL tear that’s causing instability, it’s prudent to get referred to an orthopaedic surgeon for a discussion.
No amount of online information can replace a visit with an orthopaedic surgeon to determine if you would benefit from an ACL reconstruction. This serves as a guide only.
Non-Surgical Treatment
The initial treatment for ACL tears include:
First Aid
Physiotherapy to:
- Lower your swelling
- Improve your range of motion and
- Re-activate your quadriceps to get you back walking normally.
Typically, non-surgical treatment is considered for people
- Over the age of 40
- Have a partial tear of the ACL, not causing significant instability on physical exam
- Already have significant arthritis
- Do not have any giving way in their knee with daily activities after physiotherapy
- Do not plan to return to any pivoting sports (ie sports where you need to change directions suddenly)
- Have an active infection in their knee
- Can not commit to the physiotherapy program after surgery.
Surgery
ACL reconstruction is meant for young, active patients who:
- have had known trauma to their knee causing an ACL tear
- have “giving way” from their knee or are unable to “trust” their knee when changing direction or when performing sudden movements or sports
- can commit to a physiotherapy program after surgery lasting 9-12 months
- do not have advanced knee arthritis
In ACL reconstruction your surgeon will transfer tissue from another part of your knee (“autograft”), or occasionally from a cadaver donor (allograft) to where your natural ACL was. Simply “fixing” the torn ACL back to where it was before does not typically work well, given current technologies.
Graft Choice
There are many scientific articles that debate the advantages and disadvantages of different donor sites for ACL reconstruction. Taking tissue from the Hamstrings or Patellar tendon are by far the most common practices in Canada. Dr. Cayen’s current approach is guided by the scientific literature currently available and his surgical experience.
Hamstring Autograft
Most patients prefer the hamstring tendon method since it hurts less and has fewer serious complications than patellar tendon autografts. The disadvantage of hamstring tendon autograft is that historically, it tends to loosen up a little bit with time when measured with special machines. The large majority of ACL reconstructions performed by Dr. Cayen at this time are completed using this method. A technical video on how Dr. Cayen performs a hamstring tendon ACL reconstruction can be found here.
Bone-Tendon-Bone Autograft
This method takes piece of bone from the knee cap (patella), a piece of bone from the leg (tibial tubercle) and one third of the tendon that connects the two pieces of bone (patellar tendon). It is slightly stiffer tissue than the hamstring when tested in the knee using special machines. Risks of this method include more pain in the immediate period after the surgery, pain with kneeling, and breaking (fractures of) the kneecap. In long term follow-up, patients who have had BTB autografts typically have more knee pain around the kneecap and have a higher chance of getting knee arthritis compared patients who have had hamstring autografts.
Allograft
In older patients (over 40 years old, without background arthritis), Dr. Cayen tends to use allograft ACL reconstruction. “Allograft” means that the tissue used comes from a cadaver donor. These pieces of tissue are sterilized and stored in a freezer. This graft is then used to reconstruct your ACL. As you get older, your own tendons start to get weak and thin. The allografts used are stronger than the grafts harvested from older patients.
Meniscus
Commonly there are meniscus tears that are associated with ACL tears. Dr. Cayen will address these during your ACL reconstruction surgery.
If a meniscus repair was not necessary during your surgery, (eg no meniscus work was required, or you required removal of some meniscus material) you will be allowed to put full weight on your leg after the surgery. Most patients experience discomfort in the knee as well as quadriceps weakness after ACL reconstruction. For that reason, you will likely need crutches for approximately two weeks after the procedure.
If a meniscus repair was required, you will be allowed to place only 20 to 30 pounds of pressure on your foot while walking for 6 weeks. You’ll need crutches for 6 weeks, if you have a meniscus repair.
The decision to perform meniscal trimming or a meniscus repair depends on the configuration of your meniscus tear at the time of surgery.
See section on Meniscus Tears for more information
Patient who have ACL reconstruction typically have it done under a general anaesthetic and leave hospital the same day.
The Importance of Physiotherapy after ACL reconstruction
The success of an ACL reconstruction is highly dependent on your commitment to the physiotherapy program after surgery. You are expected to have a physiotherapist guide your home-based program after your surgery. You are encouraged to see your physiotherapist within 3-6 days after your surgery for your first post-operative appointment. It’s best to book this appointment well before your surgical date.
What to expect from your physiotherapist after Surgery
Your best chance at returning to sports safely is to have your rehabilitation overseen by a physiotherapists (PT) and/or athletic therapist (AT). This means that you are under the guidance of a therapist until you return to sport (9-12 months after surgery). During your sessions, your therapists should be teaching you exercises that you can do on your own. Your therapist should observe you doing the exercises you have already been taught, correct any issues, and teach you new exercises. You are expected to do those exercises as instructed by your therapist most days of the week. The further along in your recovery, the less often you need to see your therapist.
For instance, after your surgery, a sample physiotherapy visit schedule may be:
| Time Since Surgery | Visit Frequency |
|---|---|
| Weeks 0-3 weeks | 2 times per week |
| Weeks 4-8 | Once per week |
| Months 2-6 | Once every other week |
| Months 6-9 | Once per month |
| Months 9-12 | Once every 2 weeks (sport-specific training) |
The above example demonstrates a total of 28 visits with a PT or AT over a year-long recovery. The exact frequency of your visits will depend on your progress through the recovery stages, your expectations for return to sport and the funding you may have through extended health benefits. Some patients see their physiotherapist with higher or lower frequency. The above is not meant as a policy or direct advice to any specific physiotherapist or patient.
Please see below for Return to Sport
Quadriceps Weakness
After ACL reconstruction, your quadriceps will get weak. It will be up to you, with instruction from your physiotherapist, to strengthen up your quadriceps with a diligent home-based exercise program after your surgery. Regaining normal function after your surgery will be dependent on your quadriceps strength.
Knee Stiffness
Immediately after surgery, your knee will be stiff and painful to move. It is of the utmost importance to work on moving your knee despite this discomfort in the first few days after your surgery. Doing the exercises given to you by your physiotherapist immediately after your surgery can help avoid knee stiffness.
Infection
The risk of infection after ACL reconstruction is very small. We do give you antibiotics through your IV in the operating room just prior to your surgery. The symptoms of infection include fevers, redness around the wound, persistent leaking from the wound and increasing pain. If you think you are developing an infection around your incisions, call your orthopaedic surgeon’s office as soon as possible.
Skin Numbness
Most patients experience a patch of skin numbness, about the size of their palm just to the outside of (lateral to) the vertical incision site. The skin numbness will not affect your function. This patch of skin numbness can decrease in size over months to years.
Re-Tear
Your ACL reconstruction is not indestructible and can re-tear, especially if you return to sport too soon. See Return to Sport.
Blood Clot
Although unusual, blood clots in deep veins of the leg can occur after ACL reconstruction. If you have previously had a blood clot or are taking hormonal therapy (most common type is the oral birth control pill), Dr. Cayen may prescribe a blood thinner after your surgery.
Arthritis after ACL tear.
ACL reconstruction can slow the progression of arthritis after ACL tears, but can not prevent it. See Natural History section.
Navigating the System
What you need to know.
- How to get an appointment with Dr. Cayen
If you are wondering if you need an ACL reconstruction, the first step in the Canadian Health Care System is to see your family doctor. Your family doctor will ask you questions, do a physical exam and order x-rays (if they have not already been done) to look for any broken bones. X-rays are typically normal with isolated ACL tears. If your family doctor suspects an ACL tear, then an MRI will be ordered. If you are interested in having an ACL reconstruction, your family doctor can refer you to an orthopaedic surgeon, like Dr. Cayen, who performs this procedure. You can request that your family doctor refer you to an orthopaedic surgeon of your choice.
- Your appointment with Dr. Cayen
When you see Dr. Cayen, he will ask you some questions about yourself, review your medication list, perform a physical exam on your knee and review your x-rays and MRI. If you, together with Dr. Cayen decide to proceed with ACL reconstruction, you will sign consent for surgery, attesting that you understand the risks and benefits of surgery. Dr. Cayen’s Administrative assistant will call you over the subsequent 2-3 weeks to discuss your surgical date. You may ask to be placed on a “cancellation list” if you are able to go ahead with your surgery on short notice.
- What I bring to my appointment?
1. MRI Disk : If you did not have an MRI performed at Humber River Hospital, you must bring the disk of your MRI with you to the appointment. Although Dr. Cayen may have received the MRI report from your referring physician, he needs to see the actual MRI images found on the MRI disk.
2. A pair of shorts: Dr. Cayen will need to examine your knee. He can’t do that through pants.
3. Intake Form: Print and fill out this intake form. Give it to Dr. Cayen when you meet him.
Preparing for Surgery
- General Health
1. Weight Control and Diet
• Being overweight can put excessive forces through your knee and contribute to the development of arthritis. Decreasing your weight, if necessary can improve your knee pain prior to surgery and improve the speed of recovery after surgery.
• Although exercise is important for weight control, diet is by far more important. Some things you can do to help with your diet include lowering overall portions, eating food high in protein and lower in carbohydrates, not eating after dark, not drinking beverages with calories (such as soft drinks or fruit juices) and creating a food diary. Speak to your family doctor about a weight loss program, if necessary. One resource for weight loss from the Heart and Stroke Foundation can be found here.
2. Smoking
Stop smoking at least 6 weeks prior to your surgery. Smoking inhibits bone and soft tissue healing. Smoking can increase the risk of poor wound healing and increases the risks of infection after surgery. Smoking can increase the risk of lung complications after a general anesthetic. Resources for smoking cessation can be found here.
3. Diabetes
If you have diabetes, getting your blood sugars under control prior to your surgery is important. Before your surgery, speak to your family doctor or endocrinologist about your “Hemoglobin A1c”. If it is high, it might mean that your blood sugars are not under control. Poorly controlled diabetes increases the risk of infection after knee surgery.
4. Strengthening Exercises
Seeing a physiotherapist once or twice immediately after your injury can help
• Lower your swelling
• Improve your range of motion and
• Re-activate your quadriceps to get you back walking normally.
- Discharge Planning
After ACL reconstruction, you will be discharged home the same day of surgery.
You will need:
• A ride home from the hospital, pre-arranged by you.
• A place to go after your surgery where someone can help you for a couple of days
- Assistive Devices
1. You will need crutches for 2-6 weeks after your ACL reconstruction. Bring them to the hospital on the day of your surgery, so that our physiotherapists can adjust them for you and teach you how to use them.
2. Dr. Cayen recommends the use of a cold-compression device (cryotherapy) for pain control after your surgery. This may be covered by many extended-health insurance policies. Dr. Cayen’s administrative assistant will speak to you about cryotherapy prior to your surgery.
- Day of Surgery
Do not eat or drink anything after midnight the night before surgery. You should take the medications you have been instructed to take the morning of surgery with sips of water. Do not take the medications you have been told to stop taking.
Arrive atHumber River Hospital 2 hours before your scheduled surgery. Take the Central Elevators to the 2nd floor. Go to the Surgery Registration desk on the 2nd floor. You will be registered, then get changed into a gown. (Wear briefs, not boxers. Underwear that covers the thigh will need to be removed.) You will have an intravenous line started and may be given some medications for pain and nausea. You will then see our anesthesiologist who will discuss the anesthetic. Typically, ACL reconstruction is done with a general anesthetic and possibly.
Recovery
- After Surgery
Same-day discharge from hospital
You will recover initially in the post and aesthetic care unit (PACU). You will then complete your recovery in the Surgical Day Care (SDC) unit. You will be discharged home on the same day of your surgery. You will need a ride home after your surgery.
Post-operative Splint
Will wake up with a rigid Velcro knee splint (“Zimmer splint) on. The Zimmer splint is to be used only for walking for up to 2 weeks after your surgery. You do not need to sit or sleep with it.
Ice Machine
Dr. Cayen suggests that you use an ice pack or cryo-therapy unit multiple times a day after your surgery when you are not walking, for at least 2 weeks. This will help with your pain control.
Prescriptions
You will be discharged home with a prescription for painkillers and a stool softener (if needed). You will also be given a prescription for post-operative physical therapy and a handout with a well-established rehabilitation protocol.
- Discharge Planning
After ACL reconstruction, you will be discharged home the same day of surgery.
You will need:
• A ride home from the hospital, pre-arranged by you.
• A place to go after your surgery where someone can help you for a couple of days
- Follow Up Appointments
Same-day discharge from hospital
You will recover initially in the post and aesthetic care unit (PACU). You will then complete your recovery in the Surgical Day Care (SDC) unit. You will be discharged home on the same day of your surgery. You will need a ride home after your surgery.
Post-operative Splint
Will wake up with a rigid Velcro knee splint (“Zimmer splint”) on. The Zimmer splint is to be used only for walking for up to 2 weeks after your surgery. You do not need to sit or sleep with it.
Ice Machine
Dr. Cayen suggests that you use an ice pack or cryo-therapy unit multiple times a day after your surgery when you are not walking, for at least 2 weeks. This will help with your pain control.
Prescriptions
You will be discharged home with a prescription for painkillers and a stool softener (if needed). You will also be given a prescription for post-operative physical therapy and a handout with a well-established rehabilitation protocol.
- Follow-up with Dr. Cayen After Your Surgery
You will see Dr. Cayen 1-2 weeks after your surgery. He will check your wound and make sure you are doing your home exercises. Dr. Cayen will check your knee range of motion, and see if you can do a “straight leg raise”. Your staples will be removed, if you have them. Your subsequent follow-ups with Dr. Cayen will be at approximately the 6-week, 3-month, 6-month and 9-month mark after your surgery.
All follow-up appointments occur in the Fracture Clinic at Humber River Hospital.
If you have concerns regarding your ACL reconstruction between your scheduled visits, please give Dr. Cayen’s Administrative Assistant a call.
- Wound Care
Our nurses will give you instructions on wound care. Keep the wound dry until the wound heals completely. Do not submerge the wound under water (eg in a tub or swimming pool) until the wound is completely closed (usually around 3 weeks after surgery).
- Driving
For right-leg surgery, you can drive once you are not using walking aids (eg crutches, cane etc) and are not using narcotics for pain control.
For left-leg surgery, if you are driving an automatic transmission vehicle, you can drive once you are no longer taking narcotics for pain control. If you drive a standard transmission vehicle, the restrictions are similar to right-leg surgery.
You need to feel confident that you can hit the break with good force and reaction time before you return to driving.
- Return to Work
Return to work depends on the kind of job you have. Dr. Cayen suggests working not more than 2-3 hours per day during the first few weeks after surgery and to take frequent breaks. Sitting for long periods of time after knee surgery can theoretically increase the risk of blood clots. Spend your first few weeks after surgery doing your physiotherapy and resting.
School: It is reasonable to take 1-2 weeks off school after ACL reconstruction. After that time, you will be able to attend most of your classes unless they involve prolonged standing/walking or physical activity.
Sedentary/Desk job: It is reasonable to take 2-3 weeks off of a sedentary job after ACL reconstruction. Many patients start working from home after a 1-2 of weeks (as long as they are not taking narcotics for pain).
Jobs involving walking or lifting: Typically patients can get back to an active job approximately 3 months after surgery. When you do return to work, Dr. Cayen suggests return to work gradually, with graduated hours and graduated duties over a number of weeks.
- Return to Sport
If you dutifully perform your physiotherapy after your ACL reconstruction (including a home- or gym-based strengthening program), you may be able to return to sport 10-12 months after your surgery. Patients who go back to sport too soon (before the 9 month mark) have a higher risk or suffering a repeat ACL tear.
Your physiotherapist will test out your leg strength before allowing you to return to sport. These tests include one-legged quadriceps and hamstring strength (3 rep max) and hop tests. Your operated leg needs to be 90% as strong as your non-operated leg before returning to sport.
Importantly, your physiotherapist or athletic therapist needs to train you on agility and sport-specific drills before you return to sport safely.
Dr. Cayen suggests that you get fitted for a Custom ACL Brace once your quadriceps size has recovered after your recovery. You should use your ACL brace for agility training, sport-specific training and sports up to the 2-year mark after your surgery.
- Dentist
For dental procedures, you do not need extra antibiotics above what is normally prescribed by your dentist. You should be in optimal dental health prior to your knee surgery. Infected teeth should be treated fully prior to your knee surgery. If you are approaching your scheduled regular dental cleaning, have that done prior to your knee surgery. Continue on your regular dental cleaning schedule after your knee surgery.
- Travel
Vacation travel after ACL reconstruction can be done as soon as 6 weeks post operatively. Although it is possible to travel before then, it is recommended that they be short flights and that you get up out of your seat frequently to move.
For those who must travel prior to 6 weeks after surgery, blood thinner medication may be recommended and can be discussed with Dr. Cayen or your family doctor.
Note that your self-directed exercise program should continue while you are on vacation.
DISCLAIMER: The information on this website is intended to help current and prospective patients of Dr. Cayen understand joint disease as well as treatment options available. It is also meant to provide background information to prospective patients such that their visit with their doctor is most helpful. This website is not meant to provide specific medical advice, treat or diagnose any medical condition. It is not meant to take the place of a visit with your doctor or Dr. Cayen.
About Dr. Cayen
Dr. Barry Cayen is an orthopedic surgeon at Humber River Hospital, specializing in adult hip and knee replacements, sports surgery of the knee, and trauma. He performs Total Hip Replacement Surgery using the Direct Anterior approach with a Hana table.